Long dimmed by the pandemic, lights are coming back on in symphony halls around the country. Clubs are reopening. Musicians are back on the road. But a complete industry recovery is likely more than a year away. The hardship of the last year and the uncertainty of the future are taking a toll on the mental well-being of musicians. Musicians who cannot work or who work sporadically—book an event only to have it canceled because of a COVID outbreak—not only suffer financially, they lose their creative support network.
As we enter another tenuous season of pandemic life, it’s important to find ways to maintain contact with fellow musicians and friends. Take time to make a call to a colleague or video chat with family members daily. Reach out to other musicians who can identify with your situation. Most important, achieving a more regulated emotional state takes a holistic approach.
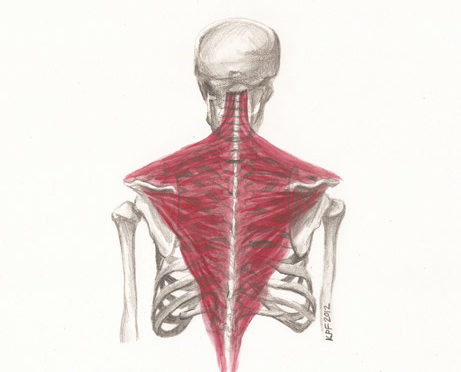
Exercise
Most forms of exercise trigger the release of “feel-good” chemicals in the brain. These mood-boosting chemicals include brain messengers such as dopamine, serotonin, and norepinephrine. Being physically active is a positive coping strategy for difficult times. Moderate exercise is a great way to refocus your energy while taking advantage of the mental and physical benefits.
Cortisol, a stress hormone released by the adrenal glands, helps your body deal with stressful situations—the “fight or flight” response. When levels of cortisol are too high for too long, it can cause a number of health issues, like weight gain and chronic disease. Exercise can help regulate cortisol levels, prompting greater resilience to acute stress.
Walk
These days we’re all looking for ways to improve our immunity, and walking seems to be a smart strategy. Research shows that moderate-intensity exercise—and walking in particular—ramps up our immune system. It increases the number of immune cells that attack pathogens in our body. Studies show substantial health benefits for people clocking between 7,000 and 10,000 steps a day.
A good walk can do wonders for your mental well-being. It’s a great stress reducer and improves mood and sleep quality. Walking is a great way to work out problems, reining in the anxiety that comes with intrusive and racing thoughts. One of the most cited studies on walking and health, published in The New England Journal of Medicine, found that those who walked enough to meet physical activity guidelines had a 30% lower risk of cardiovascular events. Pounding the pavement helps improve your range of motion and mobility because it increases blood flow to tense areas and strengthens the muscles surrounding your joints.
Tai Chi
Originally developed for self-defense, tai chi has evolved into a graceful form of exercise that’s used for stress reduction. Often described as “meditation in motion,” it’s an ideal way to help maintain strength, flexibility, and balance. There is growing evidence that this mind-body practice, which originated in China as a martial art, has value in treating or preventing many health problems. Each posture flows into the next without pause, ensuring that your body is in constant motion. The movements are usually circular and never forced. The low-impact nature of the exercises put minimal stress on muscles and joints, making it generally safe for all ages and fitness levels. It may be especially appropriate for older adults who otherwise may not exercise.
Yoga
Yoga is another mindful exercise that encompasses poses, breathing techniques, and meditation that calm and center the mind. Some yoga styles are intense and vigorous. Others are relaxing and meditative. No matter which type you choose, yoga is a great way to stretch and strengthen your body, focus your mind, and relax your spirit. According to the National Institutes of Health (NIH), scientific evidence shows that yoga support stress management, mental health, mindfulness, healthy eating, weight loss, and quality sleep. When you practice yoga in a group it can be a supportive social activity. In addition to reducing anxiety and depression, studies show that it actually makes your brain work better. When you practice yoga, your brain cells develop new connections, which strengthen memory, attention, awareness, thought, and language.
Breathe
Deep, controlled breathing, often used in mindfulness-based practices such yoga, tai chi, and qigong, is a simple technique for stress reduction, lowering the levels of cortisol. It also helps to stimulate the parasympathetic nervous system, known as the “rest and digest” system. Try this breathing exercise: Put one hand on your chest, the other hand on your lower belly, and close your eyes. Breathe in through your nose, hold for five counts, and breathe out through your mouth. Repeat as necessary.
Meditate
Meditation is a way to clear away the information overload that clouds your thoughts. A 3,000-year-old practice, meditation began as a way to deepen an understanding of the sacred and mystical forces in life. Today, it’s commonly used for relaxation and stress reduction. Even a few minutes in meditation can restore a sense of peace and can take you calmly through your day.
Wellness & Mental Health Resources
Resources are available for many types of relief. Whether you are struggling to make ends meet or need to connect with a therapist, there are organizations that support artists in need. Connect with other musicians, learn about grants or financial assistance, access free wellness content, or simply tune in to a podcast.
Backline—Connects music industry professionals and their families with a trusted network of mental health and wellness providers. www.backline.care
Sweet Relief Musicians Fund—Provides financial assistance to all types of career musicians and music industry workers who are struggling to make ends meet
while facing illness, disability, or age-related problems. www.sweetrelief.org
Black Mental Health Alliance—Develops, promotes, and sponsors trusted culturally-relevant educational forums, trainings, and referral services that support the health and well-being of Black people and their communities.www.blackmentalhealth.com
MusiCares—Provides a safety net of critical health and welfare services to the music community in three key areas: mental health and addition recovery, health (including screening and financial help); and human services (basic needs support in times of hardship). Plus programs that address affordable housing, career development, legal issues, and senior services. www.musicares.org
Check Your Head—A podcast where notable musicians share their mental health stories, experiences, and solutions, to encourage and support other musicians in finding the help that they need. Mental health experts also share their insight. The website offers free and affordable resources. www.checkyourheadpodcast.com
We Rise LA—An ongoing project of the Los Angeles County Department of Mental Health, serving the 10 million people of LA County with education and prevention programs and providing mental health-related services, offering connection, hope, recovery, and well-being. www.whywerise.la
SIMS Foundation—Provides mental health and substance use recovery services and supports for musicians, music industry professionals, and their dependent family members—through education, community partnerships, and accessible managed care. www.simsfoundation.org
The Actors Fund—Fosters stability and resiliency and provides a safety net for performing arts and entertainment professionals over their lifespan.www.actorsfund.org