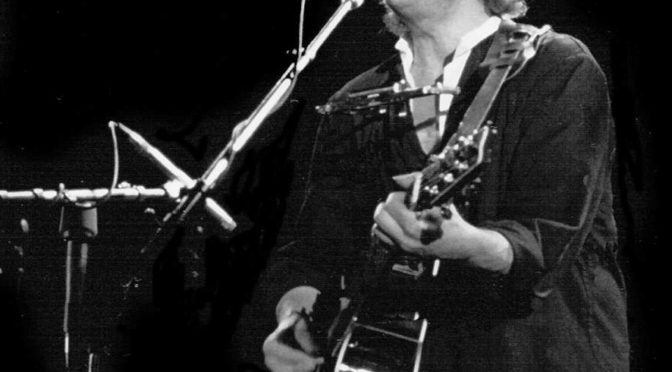
Bob Dylan never had the most beautiful voice among musician, but listening to him today it’s easy to hear his voice has gotten even coarser over the years. With the release of his newest album, Shadows in the Night, Dylan is coverings songs made famous by singers like Frank Sinatra. Not exactly the easiest songs to sing with a voice like Dylan. Seeing how getting older can affect the voice of all musicians, we’re glad Vulture reached out to otolaryngologist Dr. Milan Amin, director of the NYU Voice Center, for an explanation and more importantly, if there is any way to fix it.
Amin listened to some of the new album Shadows in the Night and compared it with Dylan’s earlier hits from the ‘60s. “The top part of Dylan’s pitch range has dropped, so he can’t access that. When he’s trying to go up in his pitch with certain words and phrases, the voice gets rough. The other thing is that his whole tone is lower.
Amin explains that vocal cords are basically muscles underneath layers of collagen and a watery substance called hyaluronic acid. “As you get older, you lose muscle bulk. The layer starts to lose both collagen and hyaluronic acid, so the entire vocal fold sags, just like skin would. How you produce voice is by having the vocal folds come in contact with each other and blowing air past them, so if the vocal folds can’t contact each other, then you can’t produce as strong a sound.”
Amin right away points out smoking can only hurt, and being in dirty bars for so long filled with smoke certainly didn’t help either. He points out that performing on a rigorous schedule for so long will wear down the vocals. He also attributes it to late night performances, lack of sleep to rest the vocals, and even eating before bed causes acid reflux which can inflame the voice-box region.
Amin makes a great analogy comparing it to a person’s joints. “You get a little ding and they don’t work like they used to. The surface lining of the vocal cords ends up getting little nicks, so they can’t vibrate like they should.”
Luckily, and very importantly, this isn’t irreparable. Unlike most other muscles in your body where you need to use them to build strength, the vocal cords can’t do that. As Amin points out, “singers would have these huge, fat vocal chords and wouldn’t be able to breathe.”
The most common solution is simple airflow exercises and behavioral modifications to make sure they aren’t damaging their voice. There are also surgical measures, as Amin explains, “You can inject materials that will essentially give the vocal folds more body. That can give you better contact between the cords and better volume. If you give the cords better volume, they can increase their pitch range.”
For all you musicians out there, take this as a warning. Listen to Dr. Amin on how to prevent voice damage. You need to protect your voice and be careful, or you will lose it. If you have an tips to share with how your keep your voice healthy, let us know in the comments below.