by Robert Fraser, President Organization of Canadian Symphony Musicians
by Robert Fraser, President Organization of Canadian Symphony Musicians
When I began my studies many years ago, I had no idea of the physical hazards of musical performance. Overuse injuries, hearing loss, unsafe performance environments—these were all very new to me and there was relatively little research or remedy in this area. I had never even heard of the drug Inderal and was astonished when my first-year music history teacher mentioned in class how many musicians took it.
Fast-forward to 2018 and there is still much work to be done. While we continually work to improve our physical safety in the workplace, dangers to our personal well-being in the form of harassment still abound, and the demands of our profession can take a toll on our psychological health. In this column, I want to draw your attention to two significant surveys, both conducted in the UK but very relevant to our position in North America.
Early last month, a few news outlets reported on survey results released by the Incorporated Society of Musicians (www.ism.org), a UK-based organization. The survey is ongoing and can still be accessed through their website. I would invite readers to look at both the survey and the report on the initial period of responses from last November. The most telling statistic, and the one that was shared in all the press articles, is that almost 60% of the respondents reported some form of sexual harassment in their musical workplace, and of those 60%, a large majority of respondents who revealed their gender were female. (The survey gives respondents the option to not reveal gender or to choose transgender; 71.71% identified as female and 10.53% chose not to identify gender.)
The report states that there were more than 250 voluntary respondents to the survey during this period. While this is not a large sample, it is telling nevertheless. It makes me wonder what the responses would be if such a survey was conducted through AFM player conference orchestras.
Another survey, done in 2016 by Help Musicians UK, was entitled Music Minds Matter (www.musicmindsmatter.org.uk) and it presents itself as being “the world’s largest known study of musicians’ mental health.” Of the 2,211 respondents, 71.1% believed they had experienced panic attacks and/or high levels of anxiety and 68.5% reported they had experienced depression—making musicians three times more likely to experience depression and anxiety than the public at-large.
Respondents to the survey listed a number of reasons for ill mental heath.
To quote directly from the summary report:
- Poor working conditions including: difficulty sustaining a living, anti-social working hours, exhaustion, and the inability to plan their time/future
- A lack of recognition for one’s work and the welding of music and identity into one’s own idea of selfhood
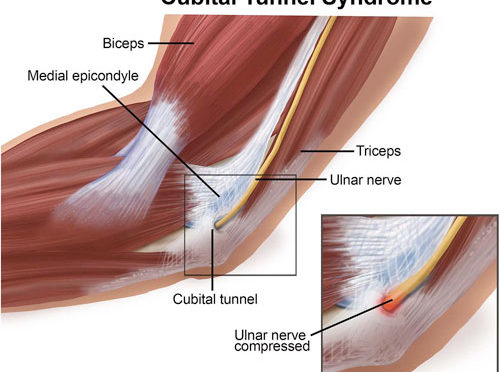
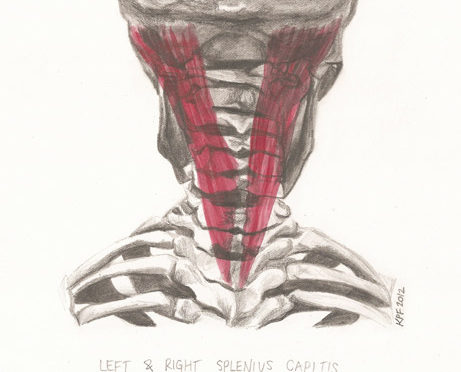
- The physical impacts of a musical career, such as musculoskeletal disorders
- Issues related to being a woman in the industry—from balancing work and family commitments, to sexist attitudes, and even sexual harassment
In October 2017, a follow-up to the Music Minds Matter survey (Phase 2) included in-depth interviews with 26 of the survey’s respondents. Again, quoting from the report, three suggested areas for change were:
- Education
- A code of best practice
- A mental health support service for those working in music
At the last OCSM Conference in August, the delegates adopted a resolution to address all three of these areas. We resolved to “encourage orchestra managers to become familiar with The National Standard of Canada for Psychological Health and Safety in the Workplace. This document can be found at the website of the Mental Health Commission of Canada. It is a daunting document (more than 70 pages), but I encourage all our members to find and download it. Point it out to your locals, your orchestra committees, and your human resources personnel. This is one area where union-management collaboration and cooperation is a must. Having research and well-documented plans for implementation will help, but the road to good mental health and safety in the workplace will not be easy.
On behalf of the 1,200 members of OCSM, I wish you all a prosperous and healthy 2018, and to my colleagues in the symphony world, an exciting second half of your season.