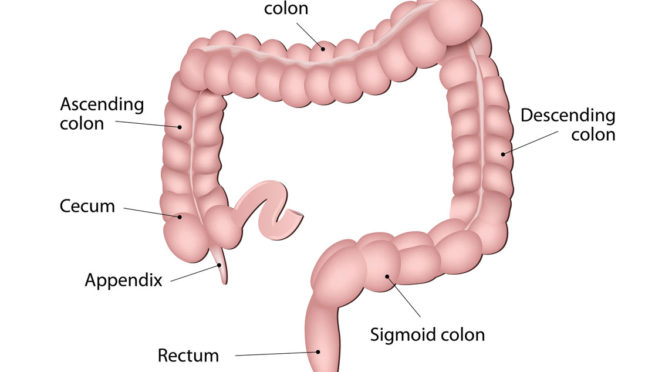
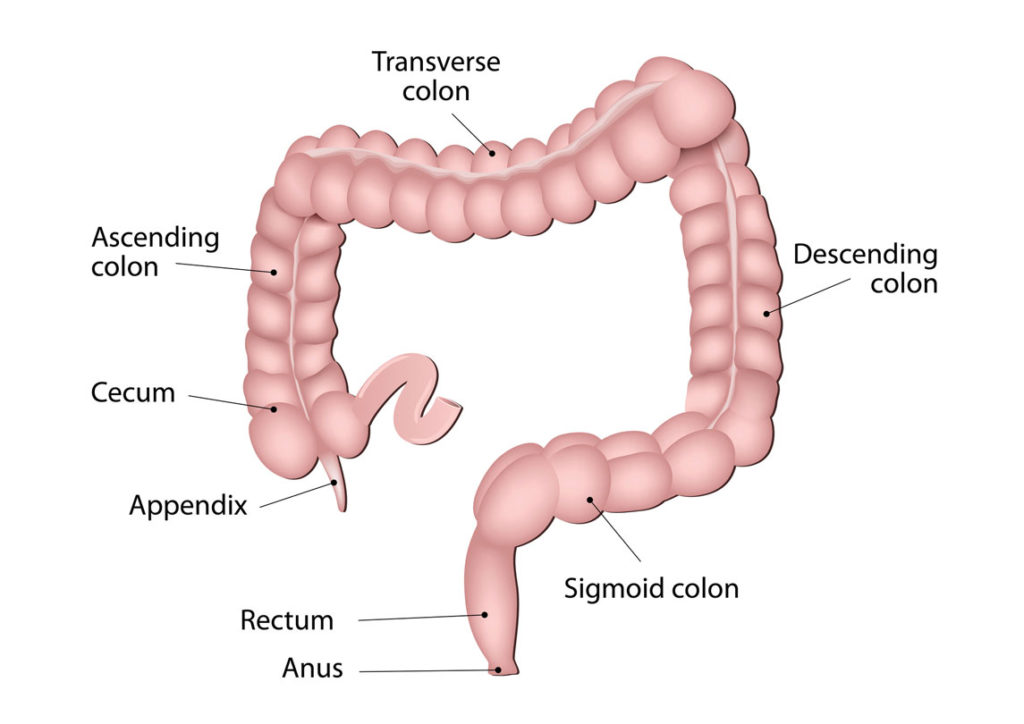
Diverticulosis is a condition in which small bulging pouches form in the lining of the digestive tract, usually in the lower part of the large intestine or sigmoid colon. Occasionally, one or more of the pouches become inflamed or infected—in which case it becomes diverticulitis, indicating an infection. An acute attack can cause severe abdominal pain, fever, nausea, and bowel irritability. Mild diverticulitis can be treated with rest, changes in diet, or antibiotics. Severe or recurring diverticulitis may require surgery. For musicians, whose careers revolve around tours, eating on the road, and sitting for long periods, diverticulosis requires vigilance.
In general, unless they have an attack, many people do not know they have diverticulosis. It is often detected incidentally, through routine colonoscopy. If this is the case, it’s important to know the symptoms of an episode, which include pain in your lower abdomen, tenderness, bloating, and cramps. If you have been diagnosed with diverticulosis, it’s advisable to enlist a gastroenterologist and see a dietitian for food recommendations.
An episode of diverticulitis may start out mild, but left untreated or unmanaged, it can escalate quickly. Subsequent episodes may become more severe. Fever is a clear indication of infection (diverticulitis), which can lead to more serious problems, such as peritonitis (caused by perforations in one or more diverticula); abscess in the abdomen; or obstruction (blockages of the intestine).
During the active stage of the infection, physicians recommend eating a low-fiber diet and drinking plenty of water. Once the infection clears, and on the recommendation of your doctor, fiber should be back on the menu.
Uncomplicated Diverticulitis
See your doctor if you have any symptoms. If it’s a mild case, she or he is likely to recommend:
• Antibiotics to treat infection, although new guidelines state that in very mild cases, they may not be needed.
• A liquid diet for a few days while the bowel heals. Once symptoms improve, gradually add solid (though low-fiber) food to your diet.
• An over-the-counter pain reliever, such as acetaminophen. This treatment is successful in most people with uncomplicated diverticulitis.
Management of Ongoing Diverticulosis
According to the American Society of Gastrointestinal Endoscopy (ASGE), diverticulosis affects half of everyone over 60 years of age in the US, though it’s rare in people under 40. As a person ages, the pouches (diverticula) in the digestive tract become more prominent. In addition, it is uncommon in certain parts of the world, such as Asia and Africa, where diets are high in fiber and rich in grains, fruits, and vegetables. For this reason, most health practitioners believe the condition is due, in part, to a diet low in fiber. A low-fiber diet leads to constipation, which increases pressure in the sigmoid colon.
Vigorous exercise appears to help lower the risk of diverticulitis. A low-fiber diet, combined with a high intake of animal fat, will likely increase the risk. While it is recommended that we consume 20 to 35 grams of fiber daily, most people only get about half that amount.
Eating vegetables and whole grains is a starting point for managing diverticulosis. Drinking plenty of water helps the body capitalize on the fiber. Doctors often recommend supplemental fiber. There are plenty of on-the-go options as well. Fiber and protein bars can supplement for days on the road when you cannot work in proper meals or regular exercise.
General guidelines include minimal use of alcohol (which dehydrates), getting regular exercise, and maintaining a healthy weight. A sedentary lifestyle is a risk factor. Desk jobs and sitting for too long are generally unhealthy: stand up every hour—move around, stretch, take a short walk. Try to fit in moderate-to-vigorous exercise during the day, like a brisk walk or a run.
Adopt a High-Fiber Diet
The best sources of fiber are fruits, vegetables, legumes, and whole grains:
• Beans, such as black beans, kidney beans
• Brown and wild rice
• Fruits, all kinds, fresh and dried, raw or cooked
• Vegetables of all kinds, raw or cooked
• Whole grain breads, cereals, and pasta
Supplements
If you have received a diverticulosis diagnosis, your doctor may also recommend that you add the following to your daily diet:
Fiber supplements: to ensure adequate fiber intake and to prevent constipation
Probiotics: as a possible measure for preventing diverticulitis
Should you avoid nuts, popcorn, and seeds?
Historically, the advice for people with diverticulosis was to avoid nuts, popcorn, corn, seeds, and seeded fruits and vegetables for fear that seeds would become trapped in the diverticula, causing inflammation. This advice is no longer considered valid. In fact, these foods are a good source of fiber. Do your research and speak to your doctor about optimal fiber intake. Also, if you have been diagnosed with diverticulosis, consider talking with a dietitian about general food guidelines for management to prevent an attack of diverticulitis.
If you have symptoms of diverticulosis or diverticulitis, you should seek immediate treatment from your healthcare provider.